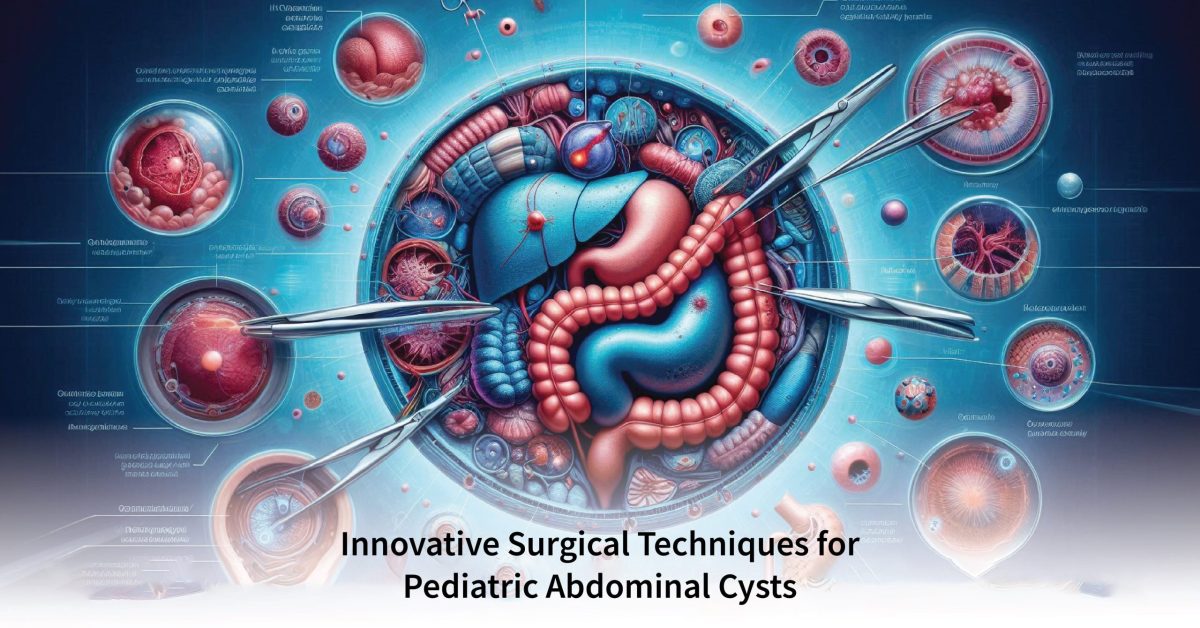
Pediatric abdominal cysts represent rare and challenging cases, which keep up the interest of those who practice pediatric surgery. The different types vary in the way they are formed, their size, and related signs. The field of surgical management has become a highly successful and extremely popular area within the last few years following improved minimally invasive laparoscopic techniques. The approach to cyst management has evolved from conventional open operations and appreciation of surgical modalities for the treatment of cysts over time with minimally invasive laparoscopic approaches. This review summarizes surgical procedures in pediatric abdominal cysts, identifying relevant findings on a well-tolerated and successful surgery regarding bleeding.
Understanding Pediatric Abdominal Cysts
These are cysts filled with fluid that may affect different parts of the abdomen, like the liver, spleen, or even intraperitoneal mesentery sites. They can be asymptomatic or cause abdominal distension and pain, nausea, or vomiting, but most often patients present with symptoms suggestive of a bowel obstruction. These cysts can be congenital or inflammatory. The right way to diagnose these cysts usually involves performing imaging tests (like ultrasound, MRI, or CT scans) that can indicate the size and location of those in the abdomen as well as reveal if they are benign.
Historical Context: Surgical Management of Pediatric Peritoneal Cysts
Traditional open techniques have been the main method for dealing with problems such as pediatric peritoneal cysts. Although this method is successful, it also has major disadvantages and complications that go with it: longer recovery time, higher pain levels, and greater risks of infection. Nonetheless, open surgery offered the benefit of direct access to and resection of cysts that were essential for preventing recurrence and complete removal.